In today’s fast-paced healthcare environment, ensuring continuous care for patients between office visits can be challenging. Enter Remote Patient Monitoring (RPM) – a game-changing technology that’s revolutionizing how we manage patient health. Let’s explore how RPM can enhance patient care and the best practices for implementation.

The Power of Continuous Care
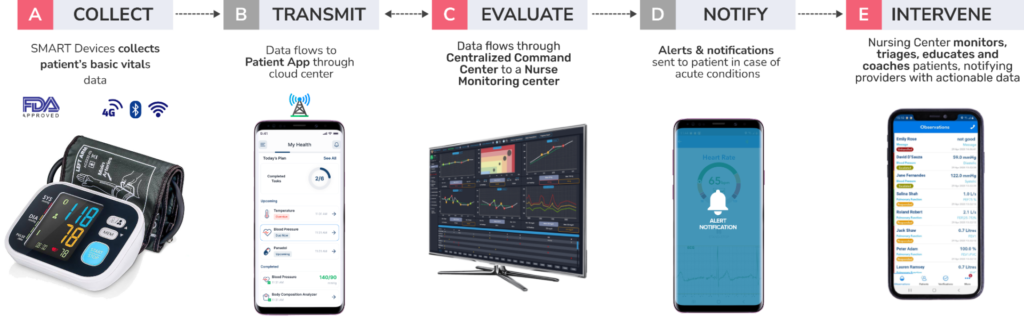
RPM allows healthcare providers to keep a watchful eye on patients’ health status outside of traditional clinical settings. By collecting and analyzing patient data in real-time, RPM bridges the gap between office visits, enabling proactive interventions and personalized care plans.
Key Benefits of RPM
- Early detection of health issues
- Reduced hospital admissions and ER visits
- Improved chronic disease management
- Enhanced patient engagement and satisfaction
Best Practices for Leveraging RPM
1. Set Clear Objectives: Define what you want to achieve with your RPM program. Is it better chronic disease management? Reduced readmissions? Improved patient outcomes?
2. Choose User-Friendly Technology: Select RPM devices and platforms that are easy for both patients and staff to use. Integration with existing systems is crucial.
3. Establish Clear Protocols: Develop standard procedures for patient enrollment, data collection, and provider response to ensure consistency and efficiency.
4. Provide Comprehensive Training: Both staff and patients should receive thorough training on using the RPM system effectively.
5. Monitor and Evaluate: Regularly assess your RPM program’s performance and make adjustments as needed.
Real-World Applications
RPM shines in managing chronic conditions like diabetes, hypertension, and COPD. For instance, daily blood pressure monitoring can help providers fine-tune medication dosages, potentially preventing complications and reducing the need for emergency care.

Overcoming Challenges
While RPM offers numerous benefits, it’s not without challenges. Addressing patient concerns about program engagement, managing data overload for providers, and ensuring proper reimbursement are key issues to tackle. Open communication and ongoing education can help overcome these hurdles.
The Future of RPM
As technology advances, we can expect to see AI and predictive analytics playing a larger role in RPM systems. These innovations will enable even more personalized and proactive care, further improving patient outcomes in other prominent chronic conditions such as Parkinson’s Disease.
Conclusion
Remote Patient Monitoring is more than just a technological advancement – it’s a paradigm shift in healthcare delivery. By leveraging RPM between office visits, healthcare providers can offer more continuous, proactive, and personalized care. As we continue to navigate the complexities of modern healthcare, RPM stands out as a powerful tool for enhancing patient care and outcomes.
Remember, the key to successful RPM implementation lies in thoughtful planning, clear communication, and a commitment to continuous improvement. By following best practices and staying attuned to patient needs, healthcare providers can harness the full potential of RPM to transform patient care.
For more detailed information, follow the link below to enhance your knowledge and take your patient care to the next level!
View our webinar here: