Every February, we see the same red ribbons and heart-shaped infographics. We’re told to “know our numbers,” but for millions of Americans living with hypertension in 2026, those numbers are nothing more than a blurred snapshot of a much larger, more dangerous story.
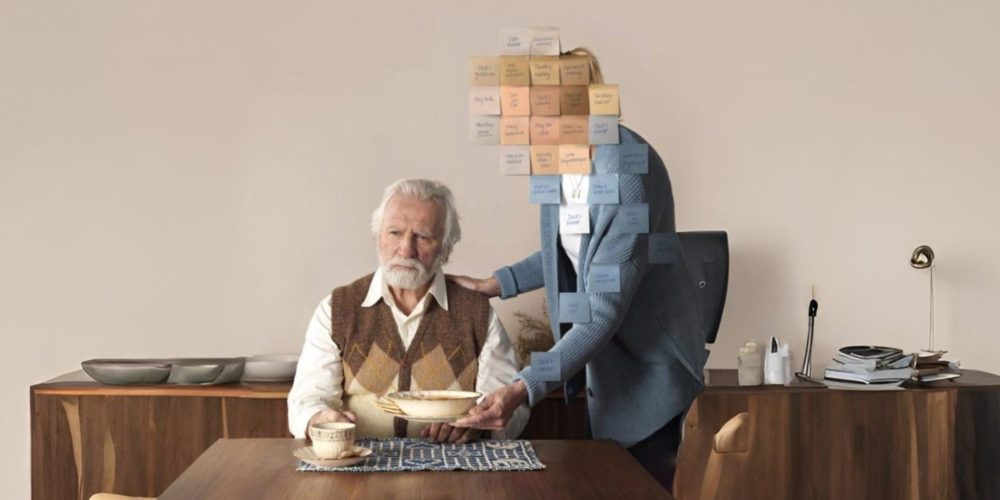
The reality of heart health is that it doesn’t happen in your doctor’s exam room. It happens in the 2,160 hours between your quarterly appointments. That is the Silent Gap, and it’s where the most significant cardiac risks reside.
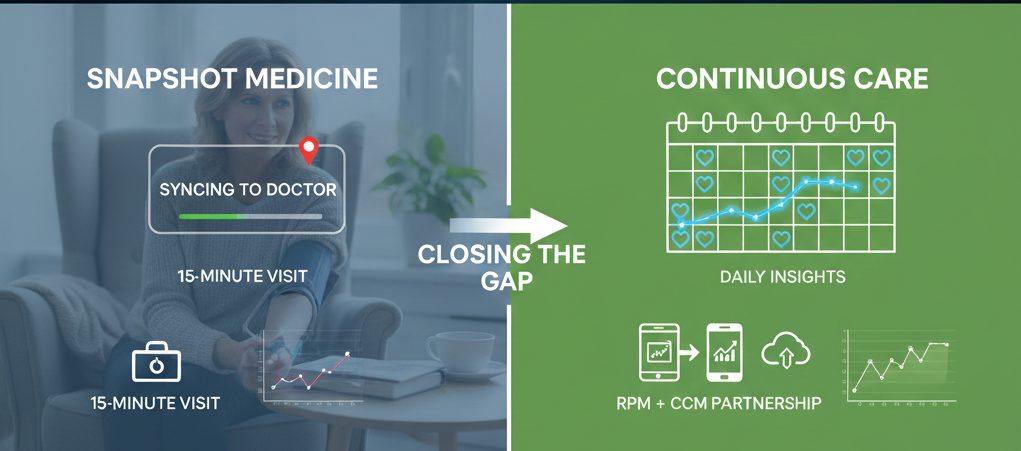
The Limitation of ‘Snapshot Medicine’
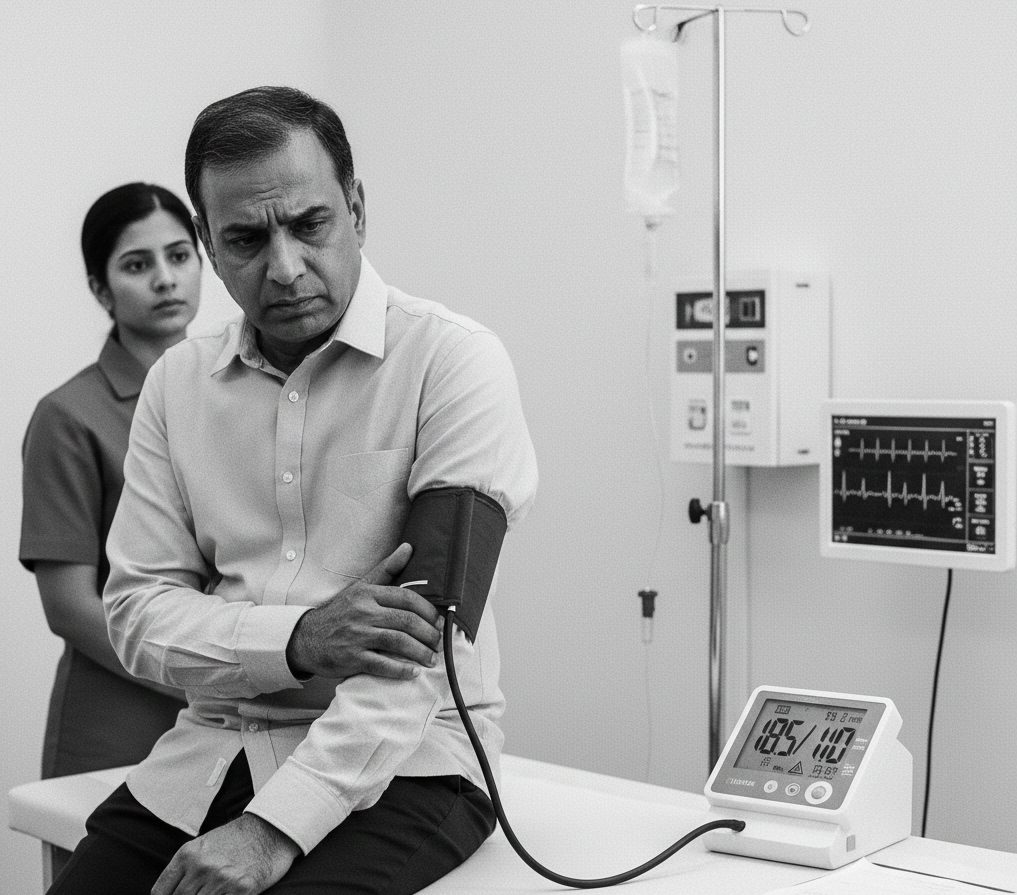
Traditional healthcare relies on episodic care. You feel a symptom (or it’s time for a check-up), you go to the clinic, a nurse takes your blood pressure, and a decision is made based on that single data point.
However, clinical research shows that White Coat Syndrome or even the simple stress of rushing to an appointment can skew blood pressure readings by as much as 15 – 20 mmHg. Conversely, some patients experience Masked Hypertension, where their pressure appears normal at the clinic but dangerously high at home.
When your care is based on a snapshot, your treatment plan is essentially a guess.
Why ‘Feeling Fine’ is the Most Dangerous Metric
In the U.S., hypertension remains the leading cause of preventable stroke and heart disease. The reason? It rarely has symptoms. You cannot “feel” your arteries hardening. You cannot “feel” your left ventricle thickening.
By the time symptoms like chest pain, shortness of breath, or headaches appear, your cardiovascular system has likely been under significant strain for years. Proactive wellness isn’t about responding to symptoms; it’s about capturing the data that precedes them.
Bridging the Gap: The Role of RPM and CCM
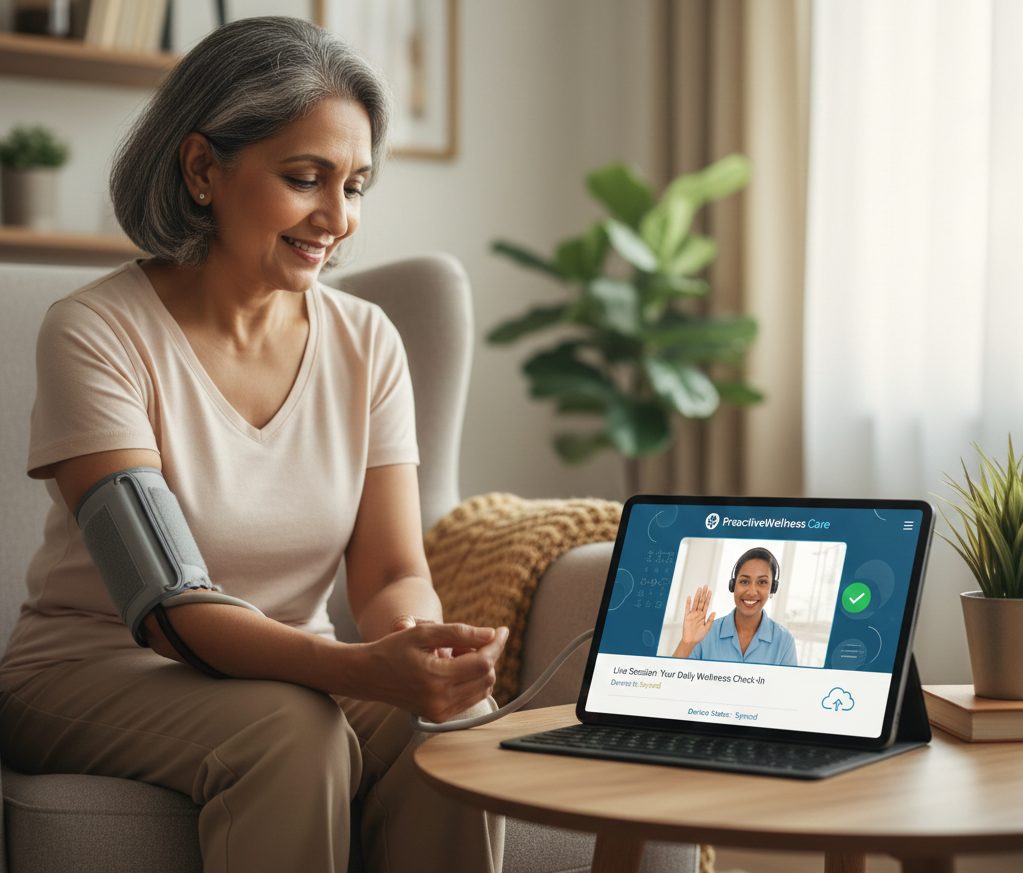
At ProactiveWellness Care, we believe that your doctor deserves a better “view” of your health. This is why we partner with medical practices to implement Remote Patient Monitoring (RPM) and Chronic Care Management (CCM).
1. Remote Patient Monitoring (RPM)
Instead of one reading every few months, RPM provides your physician with a “movie” of your heart health. Using cellular-connected devices, your blood pressure data is sent securely to your clinical team in real-time. If your numbers spike on a Tuesday at 2:00 PM, we know it—and so does your doctor.
2. Chronic Care Management (CCM)
Managing heart health involves more than just a pill. It involves medication reconciliation, lifestyle adjustments, and constant coordination. CCM provides you with a dedicated care coordinator, a healthcare professional who acts as the bridge between you and your physician, ensuring that your care plan is actually working in your daily life.
How to Move from Reactive to Proactive
If you are managing high blood pressure, you shouldn’t be doing it alone, and you shouldn’t be doing it in the dark.
Steps to take this American Heart Month:
- Request Continuous Data: Ask your primary care physician if they offer Remote Patient Monitoring through a partner like ProactiveWellness Care.
- Review the Trends: Focus on your resting averages rather than a single high or low reading.
- Engage with Your Care Team: If you have multiple conditions, ask about CCM services to help coordinate your specialists and prescriptions.
The Bottom Line
Your heart doesn’t take a break between doctor’s visits. Your care shouldn’t either. As we wrap up American Heart Month 2026, let’s commit to closing the Silent Gap.
The technology exists to keep you safe, keep you out of the ER, and keep your heart beating strong for years to come. It’s time to stop guessing and start monitoring.
Are you a healthcare provider looking to offer these life-saving services to your patients? Visit www.prowellcare.com to learn how we integrate seamlessly with your practice.